Professor Stephen Westaby DSc (Biochemistry) PhD (Bioengineering) MS FRCS FECTS FESC FICA
Professor Westaby qualified in medicine from the Charing Cross Hospital in 1972 and trained in surgery at Cambridge, in London, and the US. He was appointed in Oxford in 1986 with the remit to develop a new regional Cardiothoracic Surgical Centre. With the introduction of sub-specialities in congenital heart surgery, major thoracic aortic surgery, and advanced mechanical circulatory support, Oxford rose from the smallest to second largest unit in Britain within a decade. In 2000, Westaby was the first surgeon in the world to implant a high-speed rotary blood pump as an alternative to heart transplantation. The pulseless patient survived for eight years, by far the longest for any artificial heart recipient. Westaby continued to develop circulatory support devices and is the co-founder of the company Calon CardioTechnology, which has developed a unique British artificial heart. Gifted with ambidexterity, Westaby was a fast operator who performed 12,000 open heart and aortic procedures on both adults and children. He has received honours from the US, Russia, Japan, and China, and trained many prominent cardiac surgeons on an international basis. In addition, he has published 14 textbooks and 350 peer-reviewed papers in the cardiothoracic field. His autobiographical works ‘Fragile Lives’ and ‘The Knife’s Edge’ are award-winning best-sellers with worldwide distribution.
Having spent thirty years pioneering artificial hearts in Oxford, I was invited to deliver the opening address for the 2019 meeting of the Chinese Society for Thoracic and Cardiovascular Surgery. The date was late December and the venue was the huge Convention Centre on the bank of the Yangtze River in Wuhan.
Join the Waitlist

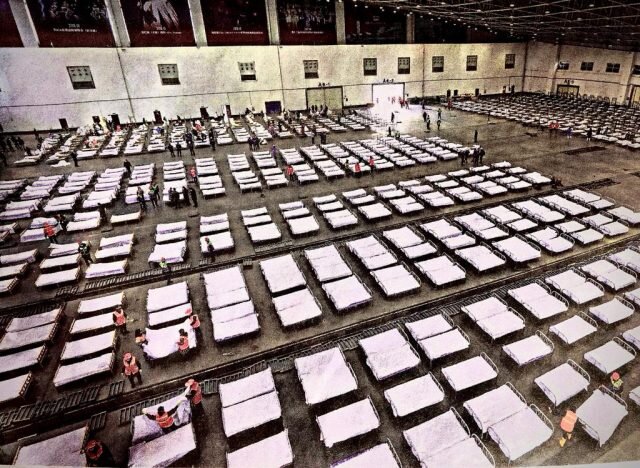
Wuhan is a bustling city of 11 million people packed into an astonishing density of high rise residential tower blocks intersected by motorways. Very little traditional Chinese culture remains on view, but the now notorious Huanan Seafood Market was just a few hundred metres from the hotel. Predictably, I had been asked to talk about the evolution of mechanical circulatory support devices as an alternative to heart transplantation. The auditorium was packed with 3000 surgeons. Only three months later, I would see a picture of the same room transformed into a vast hospital ward.

At the end of the presentation, I was asked to meet with cardiac surgeons and administrators from a couple of local hospitals. Initially, they wore face masks, common in China at the time, but soon a worrying story began to unfold. The surgeons were specifically interested in my views on the use of an external blood pumping circuit with an artificial lung to treat severe respiratory failure patients with viral pneumonia. From my book 'The Knife’s Edge' they had read about a boy dying from swine flu whom we had rescued in Oxford during the epidemic of 2009. As we talked, the Coronavirus story tentatively emerged.
A Novel Threat
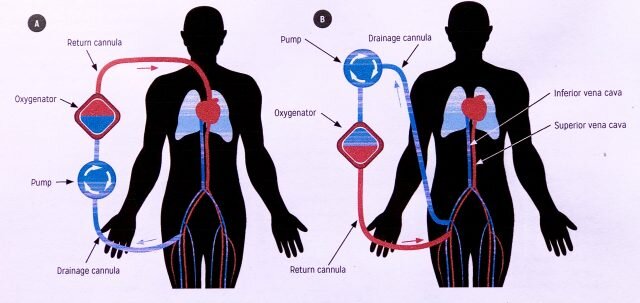
The mysterious illness was thought to have arisen nearby in around 30 patients. The main symptoms comprised fever, cough, and pneumonia. In fact, the World Health Organisation would later estimate the number of cases to be around 1000 at that point, with only a small proportion progressing to severe respiratory failure. The Wuhan Institute of Virology had identified a novel virus particle that they believed had originated in bats and then transferred to humans via pangolins in the market. Some ventilated patients had already died and the hospitals were wondering about establishing Extracorporeal Membrane Oxygenator (ECMO) beds in their intensive care units. What did I think of that proposal?
My response was an unequivocal and straightforward "Do it."
My response was an unequivocal and straightforward "Do it." Irrespective of the new infection, every cardiothoracic surgery unit should have the capacity to rescue patients from both acute heart failure or lung disease. That’s what surgeons are meant to do. I asked whether they wanted me to see the patients but was told that the issue was still too sensitive for me to visit the hospital. At that point, I was presented with an ornamental plaque and some Chinese tea and headed off for the airport to get home for Christmas.
For a few days, I remained blissfully unaware of the tragedy unfolding in China, one which spread rapidly to the rest of the world. Wuhan built a huge Covid isolation hospital in two weeks and was soon running 50 ECMO systems continuously for their sickest patients. Positive pressure ventilators were recognised to damage the inflamed lungs so strenuous efforts were made to get by with less invasive breathing assistance.

I kept in touch with my Chinese contacts during January. When home manufactured ECMO equipment was used up they imported more systems from Germany. A pattern of illness soon emerged whereby 85% of cases remained mild to moderate in severity, but some developed catastrophic lung failure around 10 days after symptomatic onset. The pathological findings were identified incidentally in lungs removed for cancer. The tissues were waterlogged and contained many white blood cells. Inflammatory markers in the blood called cytokines were dramatically raised in the critically ill.
These findings that differed from classical pneumonia reminded me of something that I discovered in America in the 1980s. In the early days of open-heart surgery, many patients suffered lung, kidney, heart and brain damage after exposure of their blood to the foreign surfaces of the heart-lung machine. Patients died after otherwise successful surgery because they became dependent on the ventilator and prolonged positive inflation pressure eventually damages the lungs. Because I had a degree in biochemistry my eminent chief Dr. Kirklin (who had pioneered the heart-lung machine) set me the task of unravelling the mechanism of what became known as the ‘Post Perfusion Syndrome’.
What I found was that certain materials which interfaced with blood in the bypass circuit triggered an inflammatory response by releasing chemicals called cytokines. These caused white blood cells to stick in the lungs and generate other damaging enzymes and free radicals. In other words, the body’s own defence systems were causing lethal injury. When I identified the culprit materials the equipment manufacturers removed them from the machine and by the 1990s the problem had abated. Some patients still reacted and we treated them with steroids or membrane stabilising agents such as zinc. Both were helpful. These fundamental discoveries saved hundreds of thousands of lives before I ever came to Oxford to develop heart surgery.
Foresight and Hindsight
When things go badly in surgery, we frequently employ a hypothetical instrument to shed light on how things could have been done better. We call it the 'retrospectoscope.' In 2016 a simulated scenario named Exercise Cygnus indicated that our healthcare system would be completely overwhelmed by a real-life pandemic. The NHS medical director at the time commented upon a serious shortage of intensive care beds, but the Government deemed the findings too sensitive to be made public. So what were the facts? In England we had just 4123 critical care beds in total (6.6/100,000 population) That is proportionally half the European average (Italy has 12.5/100,000 and Germany 29.2/100,000). But far more worrying was the corresponding number of trained staff and the relevant equipment, which accounted for the fact that the maximum surge capacity for ECMO in the whole country was 30 beds in five hospitals. If there was serious pressure, we would not have the ability to cope with it.
During January, Heathrow remained open for direct flights from Wuhan despite the unfolding pandemic. Even more, cases arrived from Italy. Covid 19 was destined to provide a defining moment for British healthcare and bioscience. Weeks into the crisis, the UK’s Covid mortality stood at 182 patients/million population versus Germany’s 42/million. Put another way, Germany had five times the critical care capability, including ECMO, and one-fifth of the deaths. Why then is our NHS frequently vaunted as the envy of the world? Taiwan, Hong Kong and Singapore did much better on China’s doorstep.
Given the distinct similarities between catastrophic Covid and the Post Perfusion Syndrome, I made the suggestion that steroids or a cell membrane stabiliser might save lives. Naturally, the prospect of giving an infected patient something to suppress the immune response was regarded as ‘off piste’ and I was ignored. ‘Pissed off’ you might say. Informing the NHS that positive pressure ventilation was ultimately damaging and that the Chinese were focusing on less invasive methods didn’t help either. The NHS had adopted a tightly regulated Covid research agenda and were not interested in the fantasies of retired old buffers.
A Race to the Bottom
By then the NHS had entered its ‘ventilators and volunteers’ phase as the Exercise Cygnus predictions unfolded. Hundreds of millions of pounds were wasted on Heath Robinson ventilators and then on Nightingale Hospitals that could never be staffed. Sir James Dyson, as we now know, negotiated directly with the Prime Minister spending £20 million to develop a device that was never used. Sadly when we approached Dyson’s company for help with battery technology for our British artificial heart we were ignored. Then the Prime Minister himself became sick and was wisely admitted to one of the few hospitals with ECMO capability.
By then it was clear that 70% of those put on a ventilator died, and so every effort was made to avoid that for Boris. Most were not so fortunate until the significance of inflammatory cytokines was recognised and steroids introduced. They are still the only therapeutic agent shown to demonstrate a mortality benefit in clinical trials. Antiviral drugs such as Remdesivir may provide modest efficacy in shortening time to recovery but do not prevent death because it is the body’s own immune system that destroys the cells containing the virus.

Needless to say, the frantic efforts to produce new ventilators proved disappointing. Instead of ordering more clinically proven machines, the Health Secretary spent £50 million with diverse manufacturing companies to produce the most basic models that could be made the quickest. According to the regulators, at least 12 of those designs were too risky to use. Indeed, the variation in deaths across different intensive care units led to the conclusion that ventilator use was contributing to mortality. So much so that the individual hospital of admission became as strong a risk factor for death as older age, pre-existing heart disease or stroke, or the presence of immunosuppression in transplant patients. Again, our intensive care units were slow to introduce the less invasive ventilatory techniques adopted in other countries because of restrictions on so-called 'clinical research.'
Good Practices, Bad Policies
In the hospitals that provided ECMO treatment, the facilities were soon at capacity. ECMO is a labour-intensive process whereby a blood pump and artificial lung take over from the patient’s own cardio-respiratory system for days or weeks until the organs recover or can be replaced. In heart surgery, sick patients who cannot separate from the heart-lung machine can be transferred to an extracorporeal support circuit with a substantial probability of survival. In Covid, as many as 75% who were otherwise destined to die have recovered. At present, the price of the equipment stands at around £100,000, whilst the daily costs amount to between £5000 to £10,000 per day.
We pioneered the technique in Oxford using charitable funds and it allowed the desperately sick to be saved. Of course, death is cheaper. Oxford no longer has it, but in an environment that publishes surgeons death rates, I argued that all cardiac units should. The centres funded to save lives are St Thomas’s and the Royal Brompton in London, then Cambridge, Leicester and Manchester. If you live in the North where I came from, the situation is troubling. Leicester and Manchester treat around 300 patients per year; Covid killed 100,000 in 2020. So even the youngest were unlikely to receive help. By comparison, the US has 264 ECMO centres treating Coronavirus.
When members of the Doctors Association were polled with the question “do you feel that the NHS was well prepared for Coronavirus?” 99.5 % of the members said “no”.
Having said all this, the clinical teams in Britain have done a fantastic job under terribly difficult circumstances. It’s the politics that are such a mess. When the virus reached our shores, the NHS had 43,000 nursing vacancies and a total of 100,000 posts unfilled. When members of the Doctors Association were polled with the question “do you feel that the NHS was well prepared for Coronavirus?” 99.5 % of the members said “no”. That hardly inspired confidence in their own working environment. Surgeons rendered redundant by the shutdown of UK healthcare adapted to being intensive care nurses, but it was not easy for the ‘Dad’s Army’ of itinerant staff to manage basic ventilators without damaging the patients. So the mortality was high, and the Nightingale Hospitals became functionally useless when incongruously they couldn’t even provide kidney dialysis.
As I’ve said, no one wanted to listen to a ‘has been’ cardiac surgeon, and who can blame them. Nevertheless, amidst enormous scepticism, Oxford achieved the world’s longest survivor of almost 8 years with any type of artificial heart, and my only heart transplant in a child still survives, with his own children 25 years later. The Calon bioengineering team has now produced a revolutionary new British artificial heart the size of a thumb which can be powered without an electric cable coming out through the skin. Our pump should be implanted into patients in the US next year as a permanent alternative to a heart transplant and obviously doesn’t need someone else to die first. All of this depends upon goodwill from the scientific community, collaboration, and funding -- each of which we have found difficult to access on home soil. Things might change when the Oxford-AstraZeneca vaccine has done its job. I sincerely hope so given the likelihood of future pandemics and the fact that Covid-19 seems to predispose to heart failure. Either way, it's clear that we need to learn important lessons from the pandemic and render our ailing NHS fit for purpose.
Join the Conversation
Join the waitlist to share your thoughts and join the conversation.
.png)